The Innate Immune System (Part 2)
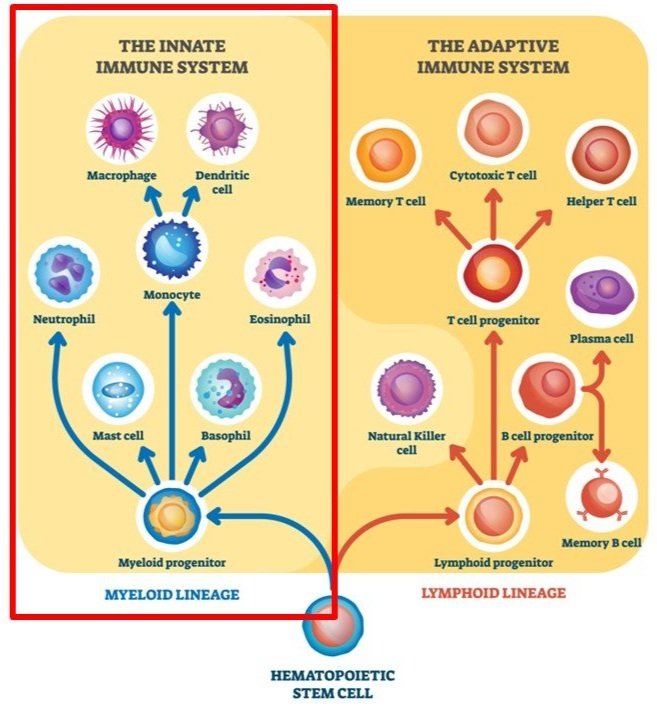
Image adapted from autobiology.net
The Innate Immune System
Like we covered in our previous blog post, the immune system consists of 3 levels of defense, with each level becoming increasingly more specific. The first level consists of the physical (ex: our skin), biological (ex: our mucus, tears, and stomach acid), and mechanical (ex: coughing, vomiting, and diarrhea) barriers that protect us. While they are effective, they are non-specific.
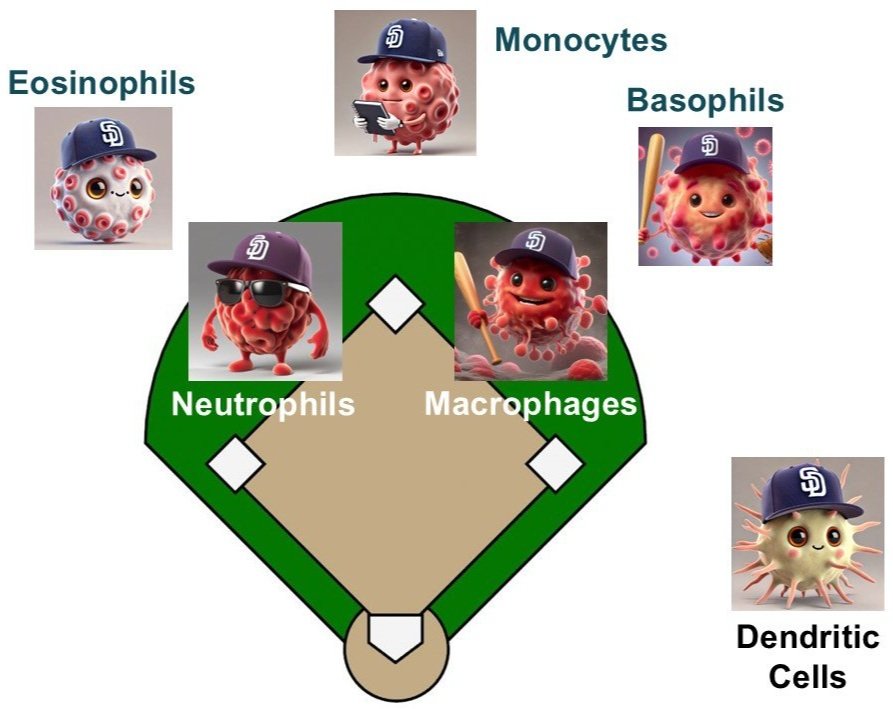
The second level of our immune defense is something called the innate immune system. The innate immune system is able to respond to a wide range of invaders once they get past our level 1 defense and enter the body. One analogy we can use to describe the immune system is that it’s like a baseball team. And in this analogy, the innate immune system is like the defensive side of the ball. In a baseball game, when you’re the home team, your defense is up first while the other team goes to bat. And what makes the innate immune system special is how quickly it can respond - even faster than the adaptive immune system (which is our level 3 defense, and in our baseball analogy, is the offense - but we’ll get to that in our next blog post).
Today, we’ll describe some of the players of the innate immune system.
Dendritic Cells (DCs)
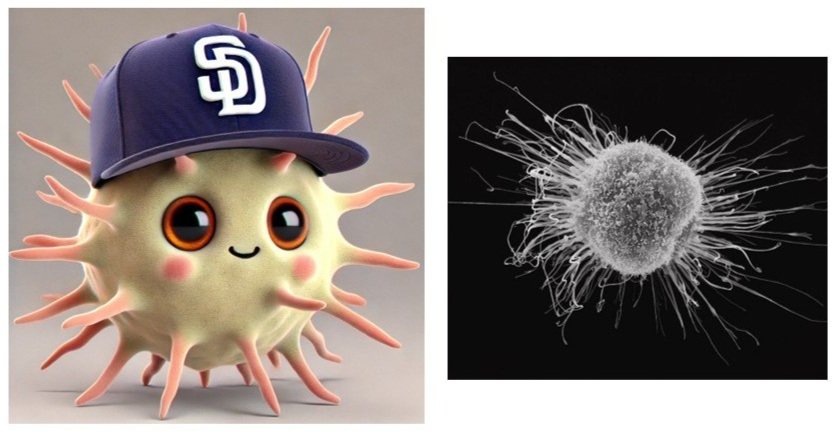
The Scouts: Dendritic Cells (DCs)
In baseball, a team will send out scouts to study their upcoming opponents before they play each other. The scouts will study the opposing team’s tendencies, like what kinds of pitches they throw in specific situations, so their team will know what to expect. In the innate immune system, this is what dendritic cells (DCs) do.
DCs are present throughout the body, especially in tissues that are in contact with our external environment (like our skin, lungs, stomach, and intestines). And just like baseball scouts, DCs scout their environment for invading pathogens (like invading bacteria and viruses). They do this by using pattern recognition receptors (PRRs), which recognize specific chemical marks found on pathogens.
Once DCs detect a pathogen, they become activated into becoming mature DCs. At the same time, they’ll capture and eat the pathogen (this process is called phagocytosis). As part of this process, they break down the pathogen’s proteins and present small pieces of them (called antigens) on their own cell surface using special receptors called MHC molecules. This is their way of showing off what they found so the rest of the immune system can see and know what to watch out for.
The DCs then travel to the lymph nodes (special meeting points in the body for immune cells, like the dugout or the clubhouse in our baseball analogy) to show off the antigens they collected to the other immune cells (primarily helper T-cells and B-cells) to activate them and tell them what to watch out for in case the body ever gets infected again with the same pathogens.
DCs are also called antigen-presenting cells for this reason: they present these antigens to the rest of the immune system, so the other immune cells know what to watch out for. This is how the immune system stays updated as we encounter different bacteria and viruses as we go through life.
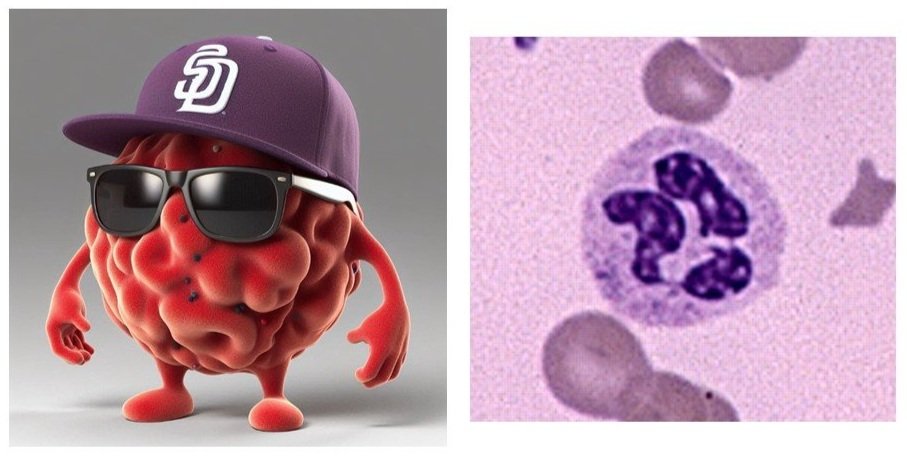
The Double-Play Middle Infielders: Neutrophils & Macrophages
In baseball, the middle infielders (the second baseman and shortstop) play a crucial role in stopping anything hit to the middle of the field. They need to be great fielders because that’s where most of the balls are hit. And if there’s already a runner on first base, they work together to try and turn the double play to end the inning.
In the same way, whenever there’s an infection, neutrophils and macrophages are often the first to respond, and they work together to stop the infection and get any invading pathogens out.
Neutrophils
Neutrophils
First up are the neutrophils. Whenever an infection penetrates past our level 1 defenses (for instance, if you get a cut on your finger), neutrophils are the first ones there. They’re our first responders, the first to the site of infection. They’re actually the main reason why pus appears yellow. And they’re everywhere - they make up 40-70% of all of our white blood cells. Here’s what they do:
They eat and digest any invading pathogens to neutralize them. They can also remove any dead or damaged cells to clean up the site (for instance, damaged skin cells on your finger where you got cut). This process is called phagocytosis (in Greek, this literally means “devouring cell”). They’re able to do this because they have specialized receptors called opsonins, which are able to recognize anything from pathogens, cancer cells, aged cells, dead or dying cells, to even things like protein aggregates like amyloid plaques (which are often associated with Alzheimer's disease).
They can also release enzymes to kill any surrounding pathogens.
They release signals to communicate with other cells (like macrophages) to recruit them to come and help battle against the infection.
Finally, neutrophils can also release web-like structures made of DNA, histones, and antimicrobial proteins which capture and kill any pathogens in the area. It’s like a spider web for the immune system. The goal is to physically trap the pathogens in the area so they can’t spread to other parts of the body.
Neutrophils have several ways they can battle infections. However, neutrophils have a short lifespan - they only live for 5-130 hours. This means that they need to coordinate with other cell types, like macrophages, to keep up the fight after they die.
Macrophages
Macrophages
Once macrophages are present at the site of infection, they work together with the neutrophils to stop the infection and start the repair and healing process. Here’s what the macrophages do:
They assist neutrophils with eating, digesting, and removing any remaining pathogens, dead cells, or debris. In fact, macrophages are professional cleaners - did you know that one macrophage can digest more than 100 bacteria before it dies? Pretty impressive!
Just like DCs, macrophages can take parts of these digested pathogens to act as antigen-presenting cells to help alert the rest of the immune system what to watch out for.
They release special signals (called cytokines) to help promote inflammation (for example, when you notice redness, swelling, or pain after you cut yourself, which is how the body isolates and removes any infections), and then later to decrease inflammation (after the infection is cleared, this helps promote the repair of any damaged tissues - like the skin where your finger was cut).
The Outfield: Monocytes, Eosinophils, & Basophils
Monocytes
Monocytes
The center fielder takes charge of the outfield and tells the other outfielders what to do and where to stand. They’ve memorized what the scouts told them and know where the opposing batters are most likely to hit the ball. And in our analogy, monocytes are our center fielders. They make up around 2-10% of all of our white blood cells, and they circulate throughout the blood for 1-3 days, before they settle down and migrate into our tissues and differentiating. Monocytes have several important roles:
Just like our other immune cells, monocytes can eat and digest bacteria, viruses, and other dead cells.
Once monocytes arrive at the site of infection, they can turn into (differentiate into) either dendritic cells (DCs) or macrophages. Both of these are important for neutralizing pathogens, controlling inflammation, and activating the rest of the immune system by acting as antigen-presenting cells. Whether the monocyte becomes a DC or a macrophage depends on the specific signals and cytokines present in that tissue.
Monocytes can also kill infected cells using a process called antibody-dependent cell-mediated cytotoxicity (ADCC), which we’ll describe later when we discuss natural killer (NK) cells in our next blog post.
Like macrophages, monocytes also release cytokines to help control inflammation - telling the rest of the immune system when to dial it up (when fighting an infection) or when to dial it down (reducing inflammation to promote wound/tissue repair).
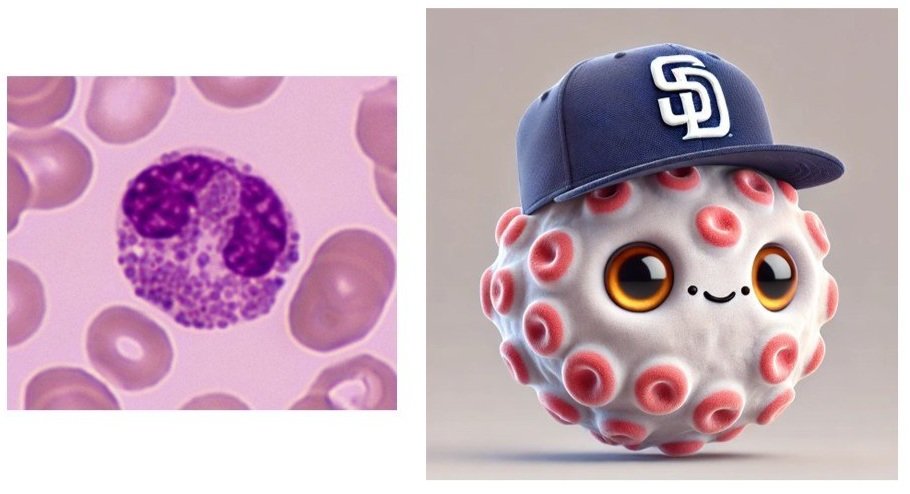
Eosinophils
Eosinophils
A great outfielder can run fast and catch anything hit towards them to get the out, including scaling the wall to rob the other team of a home run. Just like a great outfielder, eosinophils are specialized in getting the tough outs. They make up around 1-3% of our white blood cells, and they live in our tissues for 8-12 days.
First, eosinophils are really effective at combating specific kinds of infections - especially multicellular parasites, like worms. Eosinophils release toxic enzymes to kill them. Eosinophils can also release toxic enzymes targeted against certain bacteria and viruses in a process called degranulation (when eosinophils release a granule, or bag, filled with antimicrobial, toxic, or other enzymes into its surroundings).
Like macrophages, eosinophils also release cytokines to help regulate inflammation.
Eosinophils play a major role in our response to allergies. When eosinophils are activated, they release a variety of toxic proteins, including Major Basic Protein (MBP), Eosinophil Cationic Protein (ECP), and Eosinophil Peroxidase (EPO). These usually combat parasites, but they can also cause tissue damage and inflammation, which can contribute to our allergy symptoms like itching, swelling, and mucus production.
Basophils
Basophils
Finally, the last cell type we’ll be covering today - basophils!
Like eosinophils, basophils release toxic enzymes to kill parasites. Especially when there’s an ectoparasite infection like ticks, you can find a lot of basophils. They make up around 0.5-1% of our white blood cells.
Basophils release cytokines to help control inflammation. What they’re especially known for is releasing heparin, which prevents blood clotting. Heparin is important for ensuring that there is proper blood flow to the site of infection, so the rest of the immune cells can also reach the area to join the fight and work their magic.
In addition to heparin, basophils also release histamine. Basophils are very active in our allergic responses, and histamine causes our blood vessels to dilate, which helps more blood to reach the infected area. However, this also leads to more itching, swelling, and redness - this is why a lot of allergy medicines are antihistamines.
Because basophils play such an important role in simulating our inflammatory response, they are also responsible for contributing to several acute and chronic diseases, such as anaphylaxis (a serious allergic reaction that is a medical emergency), asthma, atopic dermatitis, and hay fever. Basophils have receptors on their cell surface that bind something called IgE (an antibody our body produces in response to foreign substances), which is what’s responsible for a lot of our basophils’ environmental responses (like reacting to pollen proteins).
Sign-Stealing:
As we wrap up, you might be wondering how the immune system is able to detect and recognize invading pathogens. A few years ago, the Houston Astros baseball team got in trouble for stealing signs from the opposing teams - they used spies to see what pitches the opposing team was going to throw, and then they hit trash cans to let their players know what pitches to expect. It sounds basic, but they successfully used that to beat the Dodgers in the World Series. And in a way, this is what our immune system does as well.
Many of our immune cells have specialized receptors to detect invaders. Although there are several types of receptors, they generally fall into 2 categories:
Pathogen-associated molecular patterns (PAMPs) - these are specialized receptors to detect invading pathogens (bacteria, viruses, etc.)
Damage-associated molecular patterns (DMAPs) -these are specialized receptors to detect damaged or dead cells that need to be removed
Once the cells of the innate immune system detect anything with their PAMPs or DMAPs, they jump into action and start working. And coming back to our Level 2 analogy (from our previous blog post), that’s like the patrolling security guards spotting someone trying to steal something from the stadium merch store and calling in back-ups to arrest them.
Some examples of what PAMPs and DMAPs are looking for include:
Heat-shock proteins, which are special proteins that are released by stressed cells, which can be detected by Toll-like receptors (TLRs)
ATP that gets released from damaged cells, which is detected by purinergic receptors
DNA or RNA that gets released from damaged cells, which is detected by TLRs
Then, once the neutrophils and macrophages are on the scene, the macrophages eat and digest the invading pathogens, steal small parts of those pathogens to display to the rest of their team (acting as antigen-presenting cells) so they know what’s coming up next. Everything is tightly coordinated to keep us safe and healthy!
Wrap-up
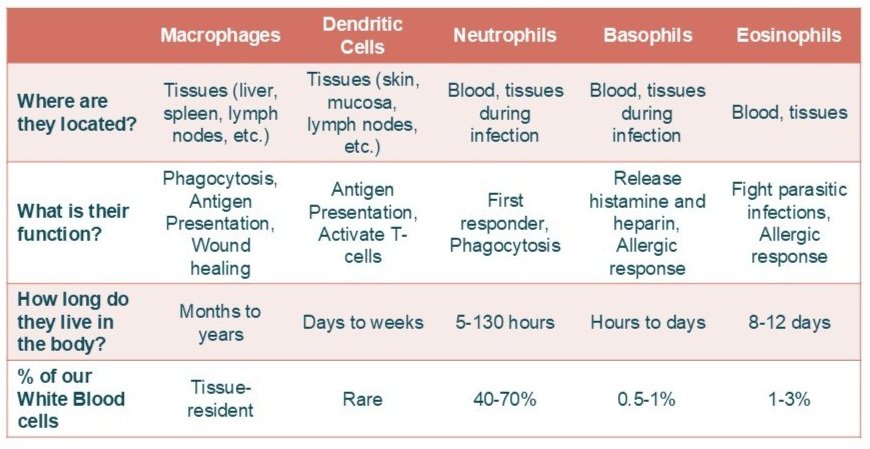
Congratulations, you made it to the end! The immune system can be very confusing with many different types of cells. Here’s a quick summary of everything we covered:
Summary of the cells we covered of the innate immune system
Our next blog post will cover the adaptive immune system (the offensive side of our team)! Stay tuned!